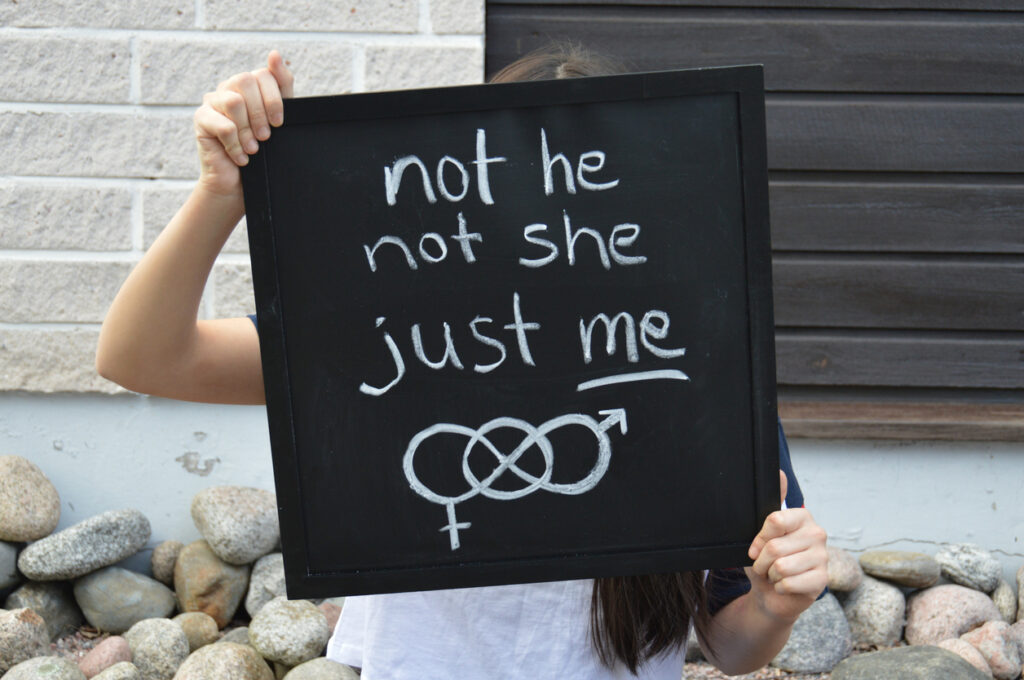
LGBTQI+ Teens, Treatment, and Inclusion
[seriesbox]Parents of LGBTQ + Teens: A Guide to Terminology and Basic Concepts You Should Know
LGBTQ+ and Transgender Teens: Using a Teen’s Chosen Name Reduces Depression and Suicide Risk
I Wish I Were Dead: Why Transgender Teens Present as Suicide Risks and What Parents Can Do[/seriesbox]In the early days of treatment for addiction and mental health disorders, ideas like equality, inclusion, and access weren’t concepts anyone considered. The first support systems for people with addiction, often called sobriety circles or temperance groups, appeared in the mid-18th century. By the mid-19th century, treatment centers – known as asylums, homes, or sanatoriums – operated on a model we abandoned at the end of the 20th century.
The conditions in mental institutions – separate from sobriety circles or temperance groups – during the 18th and 19th centuries were barbaric.
Proponents of that old model held that mental health and addiction disorders resulted from personal weaknesses, flaws in moral character, or a lack of willpower. While some gender-specific programs did exist – mainly to hide women of questionable character from society – the idea that men and women developed mental health or addiction disorders in a manner specific to their gender didn’t fit the dominant paradigm. Which, again, was firmly entrenched in the idea that character deficits drove mental health and addiction disorders, rather than biological, psychological, or other factors, such as childhood trauma or exposure to traumatic life events during adulthood.
The concept of separating men and women for evidence-based reasons was not part of the picture. And though we have no direct evidence to make the following statement, we can assume – based on the social and cultural climate of the 19th century – that consideration of the specific rights or needs of the gay, lesbian, or transgender community was never part of the picture, either.
It’s also safe to assume – based on what we know about our cultural history – that gender-specific treatment for non-binary, transgender, or teens questioning their sexuality or gender identity was not available.
The Turning Point
In the late 20th century, the treatment community learned to change.
The first gender-specific approaches appeared in the 1970s but still suffered under the weight of the fundamentally flawed moral deficiency paradigm. It wasn’t until the 1980s that mental health and addiction professionals developed the medical model of mental health and addiction disorders, which identified mental health and addiction disorders as medical conditions that responded positively to evidence-based treatment.
Under this new paradigm, treatment professionals realized that mental health and addiction disorders were just like well-known chronic conditions such as diabetes and hypertension: a combination of treatment, lifestyle change, and medication could help people heal, recover, and lead full and fulfilling lives despite their condition or disorder.
This is the paradigm we live under now. While we still have work to do to counter stigma and shake off the residual effects of the centuries-long moral deficiency paradigm, things are better now. The treatment environment, as a whole, is light-years ahead of where it was only fifty years ago. One consequence of our progress was the rise of specialized treatment for specific populations. Experts realized adults benefit from treatment tailored for adults, adolescents benefit from treatment tailored for adolescents, and children benefit from treatment tailored for children.
In addition, treatment professionals realized that in many cases – specifically in alcohol/substance abuse treatment – women benefit from treatment tailored for women, and men benefit from treatment tailored for men.
Gender Differences in Mental Health and Addiction: Prevalence and Treatment
Comprehensive meta-analyses on mental health disorders – like this one that includes data from 1.7 million people gathered over a period of 40 years – offer these insights:
- Gender differences in prevalence rates appear at around age twelve.
- They increase through adolescence and early adulthood.
- They decline during adulthood, then slowly disappear after middle age.
- Circulating hormones might play a role.
In addition, around the beginning of the 21st century, experts on addiction – which we now call alcohol use disorder (AUD) or substance use disorder (SUD) – identified the following facts. Men and women:
- May develop AUD/SUD for gender-related reasons
- Often enter AUD/SUD treatment for gender-related reasons
- May respond to AUD/SUD treatment in ways specific to their gender
However, the data on adolescents – to date – does not include evidence to support significant differences in outcomes related to gender-specific treatment for teens. There are several other things to consider when we discuss this topic:
What about non-binary and transgender teens?
What about teens who question their gender identity?
If a treatment center offers gender-specific treatment for teens, would the center segregate non-binary and/or trans teens from the gender-specific treatment groups?
We’ll address those questions in a moment. First, we’ll identify the things advocates for gender-specific treatment for adults cite as advantages.
Gender Specific Treatment: Advantages for Males
When women aren’t part of the treatment group, men increase their:
- Vulnerability
- Support for one another
- Willingness to share emotions
- Willingness to cooperate rather than compete
- Level of honesty, and deflect with jokes less often
Gender Specific Treatment: Advantages for Females
When men aren’t part of the treatment group, women increase their:
- Level of engagement in group treatment
- Willingness to share emotions
- Willingness to address issues of sex/sexuality
- Ability to bond with peers
We’ll reiterate that the bullet points above all come from what we know about gender-specific treatment for adults. We don’t doubt that some of these advantages would appear in the adolescent population, as well. However, there is no available evidence to support the idea that treatment outcomes improve for gender-specific treatment for adolescents. With that said, we also don’t discount the common sentiment that boys get along better with boys and girls get along better with girls. That statement feels true – and it may well be true – but that’s not scientific evidence from a peer-reviewed mental health journal that supports the idea that gender-specific treatment for teens is necessary or beneficial.
And it also fails to address the question of non-binary and transgender teens.
That is, unless we follow the spirit of an important component of an influential publication called “The Quality of Highly Regarded Adolescent Substance Abuse Treatment Programs” and its follow-up publication, “Treating Mental Health and Substance Use Disorders in Adolescents: What Is on the Menu?”
In their outline of the ten essential components of highly regarded mental health and substance abuse treatment programs, experts on adolescent mental health identify a component that speaks directly to the topic of this article:
Culture, Gender, and Identity Sensitivity:
Treatment center staff understand and serve the needs of their entire population. Clinicians understand and have training in treatment practices specific to females, males, LGBTQI individuals, and cultural/ethnic minorities.
Let’s take a look at how treatment centers can apply culture, gender, and identity sensitivity in the treatment context.
What is Cultural Competence With Regards to LGBTQI+ Adolescents?
A paper published in 2021 addresses this question specifically. The paper – an excerpted chapter from a new book – is called “Cultural Competence in the Care of LGBTQ Patients.” The authors lay out in clear terms what cultural competency for the care of members of the LGBTQI+ community entails. If a treatment center were to offer gender-specific treatment for teens – the effectiveness of which is not yet supported by clinical data – and include transgender teens, non-binary teens, and teens questioning their gender identity, the treatment center would need to create an environment that includes all the components we’ll list in a moment.
Before we offer this list, we will recognize there are instances of single-gender groups that would benefit the adolescents involved. People with a history of sexual trauma, for instance, often experience better treatment outcomes when an individual of the gender of their abuser is not present or part of their treatment experience.
Also, a recent paper about the transgender experience in addiction treatment, called “Transgressing Gender Norms in Addiction Treatment: Transgender Rights to Access Within Gender-Segregated Facilities.” Study authors point out transgender people in gender-segregated treatment facilities experience “enacted and felt stigma” which can “result in negative treatment experiences.”
In order to support transgender individuals, organizations should:
“…dismantle institutional policies around gender segregation that alienate and discriminate against transgender populations. This includes policies that conflate sex and gender, designating transgender individuals to facilities and program components on the basis of their birth sex as opposed to identified gender.”
When an organization does those things, it increases the likelihood transgender individuals will feel welcome, supported, and participate and adhere to treatment at higher rates.
That’s specific to the transgender members of the LGBTQI+ community. Now we’ll offer the list of treatment factors that demonstrate “culture, gender, and identity sensitivity” for all members of the LGBTQI+ community. Reminder, this list is from the piece we link to above, “Cultural Competence in the Care of LGBTQI+ Patients.”
LGBTQI+ Teens: How Treatment Centers Can Create a Welcoming, Supportive Environment
Treatment centers can:
- Make it clear in marketing material and website content that they accept members of the LGBTQI+ community with open arms
- Employ staff experienced in discussing sexual and gender orientation
- Hire members of the LGBTQ community as clinicians and staff
- Always refer to an individual by their chosen name
- Always use an individual’s pronoun of choice
- Hire staff and clinicians who celebrate diversity and are enthusiastic about working with all teens, regardless of gender, sexuality, or orientation
- Make transgender an option on all intake forms and relevant paperwork
- Support the LGBTQI+ community by participating in awareness days and months. Specifically, by “displaying symbols and posters of ethnically and racially diverse transgender or same-sex couples” on LGBTQ Pride Day and National Transgender Day of Remembrance
- Provide LGBTQI+ inclusive reading material in waiting rooms and common spaces
- Prioritize staff and clinician continuing education on topics and treatment practices relevant to the LGBTQI+ community
While these details mean everything – literally everything – to a member of the LGBTQI+ community, and transgender people in particular, the general message is this:
Where inclusivity is concerned, it’s not enough to talk the talk. To support members of the LGBTQI+ community, treatment centers must also walk the walk. In other words, their policies need to reflect their priorities. If their priorities are to support all teens – including transgender teens – then their daily practices must reflect the priorities determined by their policies.
That means implementing everything we list above, and – until evidence shows otherwise, and with very few exceptions – it means that gender-specific treatment for teens may be unnecessary, and lead to the exclusion of specific members of the LGBTQI+ community.